PAKO
Cancer patients are confronted with disease-related challenges. The extent to which those affected feel able to cope with these challenges and the extent to which they would like support to strengthen their competence has been little researched to date. Patient competence (PC) is defined as “the ability to deal with the tasks that arise from cancer, to determine and pursue one's own needs and goals, and to use support from caregivers and the healthcare system (Weis & Giesler, 2008). Following the health literacy framework by Parker and Ratzan (2010), this can be understood as the interplay of personal competencies and the respective situational demands or the complexity of the systems within which these must be realised. The project aimed to gain insights into the development of PC across the disease course in women with breast or gynaecological cancer.
Research question. The following questions were investigated: (F1) What challenges in the domains of information acquisition, psychological distress, and physical complaints and long-term consequences are the women affected confronted with? (Q2) Do they perceive themselves as competent to overcome these challenges or to use support? (Q3) In which domains and in what form would they like support to strengthen their competencies?
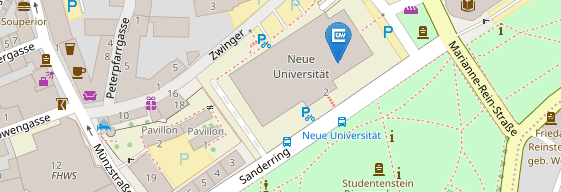
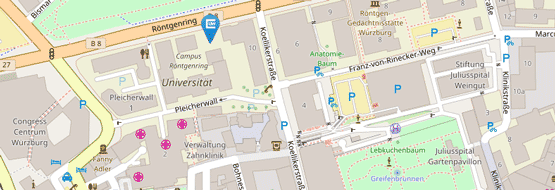
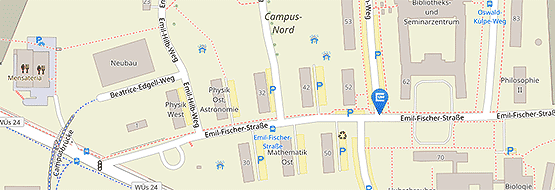
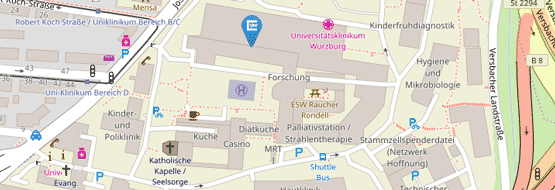
Methodology. A mixed-methods design with two consecutive study parts was implemented in the project. In study part 1, 55 guided interviews were conducted with affected women in acute hospitals (after surgery), at the end of inpatient rehabilitation, or from self-help groups. Interviews were analysed using content analysis. Based on these qualitative research results, a questionnaire was designed to assess 25 challenges and subjective coping competencies and support needs. In study part 2, a prospective cohort study was conducted with n = 120 patients and questionnaire surveys at the end of acute therapy (t1) and after 6 and 12 months (t2, t3).
Results. The most common moderate to severe challenges (at least 50%; t1 to t3) were related to coping with psychological distress (e.g., dealing with fears and insecurities, coping with the cancer diagnosis) and dealing with physical complaints (e.g., dealing with reduced capacity). The proportion of women who subjectively experienced competence in dealing with these individually relevant challenges is between 43% and 75% at the end of acute treatment. These proportions increase throughout the disease for most challenges (t3: 52-88%). 47% of patients indicated at least one (additional) need for support across all domains (t1; median = 0.0, IQR 0.0-3.0). The proportion of women with support needs is heterogeneous over time.
Areas with particular relevance concerning the three components are: dealing with fears/insecurities; coping with cancer diagnosis; dealing with reduced capacity; reducing physical complaints; paying attention to relaxation; being physically active regularly; understanding and evaluating information; using information for decision-making; access to further treatments and support offers; return to work.
Conclusion. The results illustrate the diversity and change in individual challenges, subjective coping skills, and support needs up to one year after acute treatment. Offers to strengthen personal competencies should exist in the longer term and be accessible according to individual needs. PC can be promoted via several components. Their individuality and the complexity of their interplay emphasise the relevance of empowerment and patient-oriented care.